Sleep stands as a cornerstone for both physical and mental health, underpinning our daily well-being and functioning. It rejuvenates our body, aids in the repair of cells, and consolidates our memories, playing a critical role in emotional regulation and cognitive processes. As we delve into the intricate relationship between sleep and mental health, the focus sharpens on understanding how disruptions in sleep patterns can significantly impact mental health, particularly in relation to depression. This exploration reveals the complex ways in which inadequate or disturbed sleep contributes to the development and exacerbation of depressive symptoms, highlighting the necessity of addressing sleep within the context of mental health treatment.

Recognizing this vital connection, Lumina Psychiatry stands at the forefront of incorporating sleep management into the broader spectrum of mental health care. By integrating sleep assessments and targeted interventions into their treatment plans, Lumina Psychiatry not only addresses the symptoms of mental health conditions like depression but also targets one of their root causes, offering a more comprehensive and effective approach to mental health care.
This proactive stance underscores the importance of sleep in achieving and maintaining mental health equilibrium, marking a pivotal step towards holistic patient care.
The Importance of Sleep for Mental Health and Well being
Understanding Sleep and mental health
Sleep serves as a fundamental pillar for mental well-being, influencing every aspect of our health. When we understand sleep cycles, we uncover their critical role in supporting brain function. These cycles, consisting of different stages, play a vital role in processing memories, healing the brain, and rejuvenating the mind. However, when sleep deprivation enters the picture, it wreaks havoc on the body and mind, impairing cognitive functions, emotional resilience, and overall physical health.

Sleep and Emotional Regulation
The relationship between sleep and emotional regulation further underscores sleep’s importance. Adequate sleep directly contributes to mood stability and emotional well-being. It allows the brain to process emotional experiences and regenerate, ensuring that we can handle stress and challenges more effectively. Conversely, poor sleep patterns can heighten stress and anxiety levels, directly feeding into the cycle of depression. This negative impact on emotional regulation demonstrates how essential quality sleep is for maintaining health and combating disorders like depression. Ensuring a good night’s sleep thus becomes a critical strategy in promoting mental resilience and emotional stability.
Unraveling the Connection Between Sleep and Depression
Sleep Disorders and Their Role in Depression
Delving into the complex relationship between depression uncovers a crucial aspect of mental health care. Common sleep disorders like insomnia and apnea do not merely disrupt rest; they significantly contribute to the onset and severity of depression. These disorders create a turbulent environment for the brain, impairing its ability to recover and regulate emotions effectively. With insomnia affecting about one-third of the adult population at some point in their lives, and a notable percentage of these individuals also battling depression, the statistical overlap points to a deep, intertwined connection.
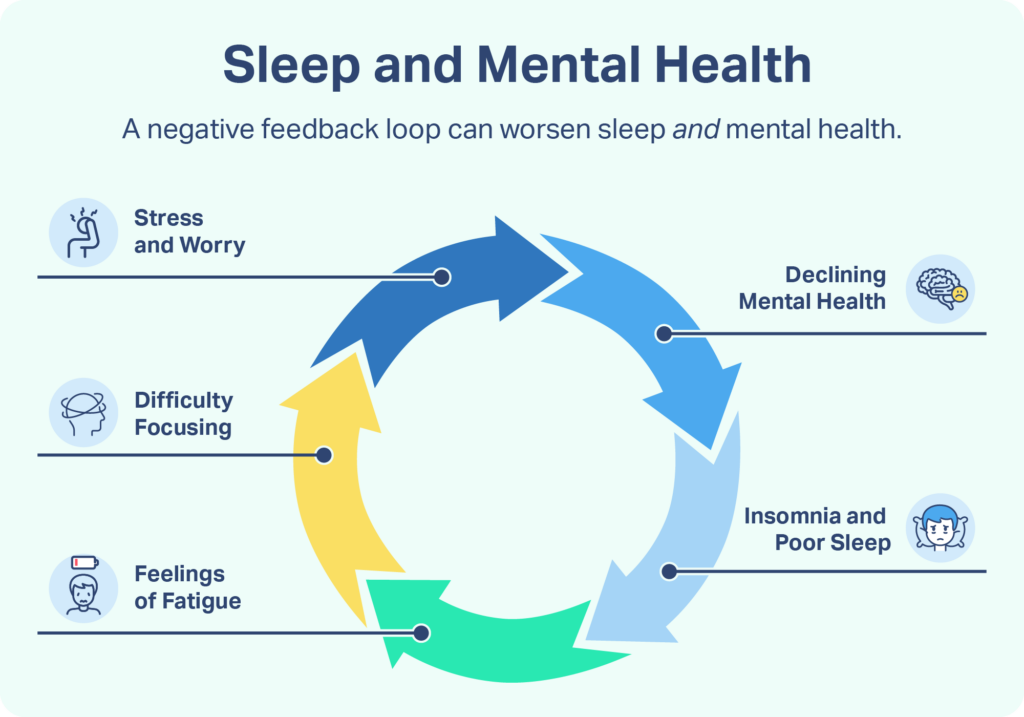
The Bidirectional Relationship Between Sleep and Depression
This relationship between sleep disorders and depression is not one-sided; it is, in fact, bidirectional. Depression often paves the way for sleep disturbances, creating a vicious cycle that can hinder treatment and recovery. Individuals with depression may find their sleep pattern fragmented, struggling with either too much sleep (hypersomnia) or too little (insomnia). This disruption in sleep exacerbates depressive symptoms, making it harder to find relief and advance in treatment. Acknowledging and addressing this cycle is pivotal in devising effective treatment strategies. By understanding the mutual influence of sleep and depression, healthcare providers can tailor interventions that target both aspects, offering a more holistic approach to recovery and well-being.
The Science Behind Sleep and Mental Well being
Neurochemical and Brain Structure Changes
Sleep profoundly influences neurochemistry and the brain’s structures that govern mood regulation. As we cycle through various stages of sleep, our brain undergoes restorative processes essential for emotional resilience and cognitive clarity. Particularly, REM sleep plays a critical role in processing emotions and consolidating memories, allowing us to navigate our emotional experiences more effectively. This stage of sleep acts as a neural cleanser, resetting the brain’s emotional compass for the coming day.
Hormonal Imbalances and Sleep
Moreover, sleep maintains a delicate hormonal balance crucial for mood stabilization. It regulates cortisol, the stress hormone, ensuring that its levels do not escalate and lead to increased stress and anxiety. Simultaneously, sleep boosts the production of melatonin, which not only aids in sleep regulation but also promotes a calming effect on the brain. This hormonal regulation is essential for warding off mood disorders and maintaining mental health. Disruptions in this balance can lead to significant mood fluctuations, highlighting the importance of consistent, quality sleep in preserving mental well-being.
Lumina Psychiatry’s Approach to Integrating Sleep Management in Depression
Holistic Treatment Plans
Lumina Psychiatry champions a comprehensive approach to care by seamlessly integrating sleep management into its holistic treatment plans. This innovative strategy acknowledges the profound impact of sleep on mental well-being and leverages a combination of therapy, medication, and sleep regulation techniques to address the unique needs of each patient. The emphasis on personalized treatment plans ensures that every individual receives care that not only targets their mental health challenges but also aligns with their specific sleep-related issues, fostering a more effective and sustainable path to recovery.
Innovative Therapies and Support Systems
At the heart of Lumina Psychiatry’s innovative approach lies a selection of cutting-edge therapies, among which Cognitive Behavioral Therapy for Insomnia (CBT-I) stands out for its effectiveness in treating sleep disturbances that often accompany mental health conditions. Beyond therapy, Lumina Psychiatry places a strong emphasis on support systems and education, empowering patients to develop healthier sleep habits that contribute to their overall mental health. This multifaceted approach not only addresses the immediate symptoms of mental health disorders but also lays the groundwork for long-term well-being, underscoring the integral role of sleep in the broader spectrum of mental health care.
Conclusion
The intricate link between sleep and mental health, especially concerning depression, underscores the critical need to address sleep disturbances within the framework of comprehensive mental health care. Recognizing and treating sleep issues not only aids in the direct management of depressive symptoms but also enhances the overall effectiveness of mental health treatments. Clinics like Lumina Psychiatry play a pivotal role in this advancement, pioneering the integration of sleep management into mental health care. Their efforts illuminate the path toward more holistic and effective approaches to mental wellness, affirming the essential nature of sleep in the pursuit of mental health recovery and resilience.
“Ready to transform your sleep and boost your mental well-being? Visit our website now to learn more about our groundbreaking approach to integrating sleep management into mental health care. Take the first step towards a healthier, happier you today!”